What happens with endometriosis? 4 major symptoms you need to know—get the right treatment and pregnancy will no longer be a worry!
When you hear the term “endometriosis,” do you feel a little nervous, or perhaps don’t even know what this condition is? In fact, it is a common yet often overlooked gynecological issue that can cause more severe menstrual cramps, irregular periods, and even affect future fertility plans. Many patients only realize the problem after failing to conceive despite actively trying.
Actually, as long as it is diagnosed early and properly treated, endometriosis does not mean you can’t get pregnant. Curious about what happens with endometriosis? Keep reading to find out more!

What is endometriosis? What happens with it?
Endometriosis refers to a common and destructive gynecological condition, estimated to affect about 10–15% of women of childbearing age worldwide. Under normal circumstances, the endometrium thickens along with the menstrual cycle and is eventually discharged through menstruation.
However, in patients with endometriosis, endometrial-like tissue appears abnormally outside the uterine cavity, most commonly on the ovaries, fallopian tubes, and pelvic peritoneum. This can lead to repeated inflammation, adhesions, pain, and even affect the ability to conceive.
Common sites of ectopic endometrial tissue include:
-
Ovaries (may form what is known as a "chocolate cyst")
-
Fallopian tubes
-
Pelvic peritoneum
-
Bladder, intestines, and other nearby organs (less common)
Although the exact cause of endometriosis has not yet been fully clarified by the medical community,the main medically recognized possible causes include:
retrograde menstruation (menstrual blood flowing backward through the fallopian tubes into the pelvic cavity),genetic predisposition (a higher risk for those with a family history),and immune system abnormalities (which fail to effectively eliminate ectopic endometrial tissue).
These abnormal tissues undergo repeated bleeding and inflammation with each menstrual cycle,leading to chronic pelvic pain or dysmenorrhea,and may affect ovarian reserve and embryo implantation.
👉 Related reading:Endometriosis and Infertility – Pregnancy Complications and Infertility Treatment Options
What are the symptoms of endometriosis?
Endometriosis symptoms vary greatly from person to person. Some only experience mild discomfort, while others suffer from severe pain that affects daily life. The most common clinical symptoms include:
1. Severe menstrual pain (dysmenorrhea)
Menstrual cramps are the most common early symptom of endometriosis. The pain may start before the period, last throughout, and even continue afterward. It is often described as a dull or stabbing pain in the lower abdomen, waist, or deep in the pelvis. In severe cases, painkillers are needed to function through daily life.
2. Chronic pelvic or lower abdominal pain
In addition to menstrual pain, some patients experience persistent or intermittent lower abdominal discomfort outside of their period, especially after sitting for long periods, during bowel movements, or after exercise. These symptoms are often mistaken for digestive or urinary tract issues, which may delay diagnosis.
3. Pain during intercourse
Many patients with endometriosis experience deep pelvic pain during intercourse, especially with deep thrusting. This occurs because ectopic endometrial tissue stimulates pelvic nerves or because adhesions have caused the uterus and ovaries to shift. Over time, this may affect intimate relationships and quality of life.
4. Abnormal menstruation and changes in menstrual flow
This includes irregular cycles, prolonged periods, excessive bleeding, or mid-cycle spotting. These symptoms may result from hormonal disruptions and abnormal responses of the endometrium. Some patients may even develop anemia.
What are the diagnostic methods for endometriosis?
Because the symptoms of endometriosis are varied and often resemble those of other gynecological conditions—such as menstrual cramps, pelvic pain, or infertility—it is often overlooked or misdiagnosed. Therefore, the diagnostic process is very important and typically involves the following steps:
-
The doctor will conduct a detailed review of the patient’s symptoms, menstrual history, and family medical history.
-
A gynecological examination will follow, using pelvic palpation to perform an initial assessment for abnormalities.
To more accurately evaluate the condition, the doctor may recommend an ultrasound to check for any abnormal lesions in the ovaries and pelvic cavity. However, a definitive diagnosis typically requires a laparoscopy. This is a minimally invasive surgical procedure performed under general anesthesia, allowing direct visualization of the pelvic area through a laparoscope. Tissue samples can also be collected for pathological analysis to confirm the final diagnosis.
Causes and risk factors
The exact cause of endometriosis is still not fully clear, but the commonly accepted contributing factors include:
-
Retrograde menstruation: During menstruation, some blood may flow back through the fallopian tubes into the pelvic cavity, leading to ectopic growth of endometrial tissue
-
Genetic factors: Women with a family history are more likely to develop the condition
-
Immune system abnormalities: When the immune system fails to clear ectopic endometrial cells effectively, these cells may continue to grow and cause inflammation
Endometriosis may lead to pelvic adhesions, poor fallopian tube function, and decreased egg quality, thereby affecting fertility.

Diagnostic Methods for Endometriosis
The symptoms of endometriosis are diverse and often resemble those of other gynecological conditions, such as menstrual cramps, pelvic pain, or infertility. As a result, the condition is frequently overlooked or misdiagnosed. Common diagnostic procedures and methods include:
|
Item |
Explanation |
|
Detailed Medical History and Symptom Assessment |
The doctor will ask about menstrual cycles, characteristics of menstrual pain, pain during intercourse, difficulties with bowel movements or urination, and family history. These help with the initial evaluation of whether the patient may have endometriosis. |
|
Gynecological Examination |
A pelvic exam is performed to assess whether there are any abnormalities in the uterus, ovaries, or surrounding tissues, such as masses, tenderness, or adhesions. |
|
Imaging Studies |
Includes two types: 1. Transvaginal Ultrasound – Used to check for ovarian cysts (e.g., chocolate cysts) or structural abnormalities. 2. Magnetic Resonance Imaging (MRI) – Suitable for assessing deep endometriosis or complex lesions, providing clearer images to support diagnosis and treatment planning. |
|
Laparoscopic Examination |
Considered the gold standard for diagnosis. A minimally invasive procedure that allows direct visualization of the pelvic cavity, confirming the location and extent of the lesions. Tissue samples can also be collected for pathological analysis. |
|
Blood Test |
Measures serum CA-125 levels, which can assist in diagnosis. However, it is not a specific indicator and is mainly used as a reference. |
Endometriosis not only affects a woman's quality of daily life, but may also significantly impact fertility.
Ectopic endometrial tissue can lead to pelvic adhesions, blocked fallopian tubes, and impaired ovarian function, all of which reduce the chances of conception.
According to research, approximately 30% to 50% of women with endometriosis may face infertility issues.
Women aged between 25 and 40, especially those experiencing worsening menstrual cramps, irregular cycles, or long-term infertility, are advised to undergo early examination to ensure their fertility plans remain on track.
Common Questions About Endometriosis
Q1. Can endometriosis affect natural conception?
Yes! Endometriosis may impact natural fertility because ectopic endometrial tissue can cause fallopian tube blockage or decreased ovarian function, hindering the normal conception process.
Women who plan to have children are advised to seek medical evaluation early.
Related Reading: What Is The Best Fertility Treatment for Endometriosis?
Q2. What fertility assistance options are available?
For patients facing fertility challenges caused by endometriosis, there are several assisted reproductive options:
-
Egg Freezing: Preserves eggs for future use. Ideal for women who aren’t ready to conceive yet but want to retain fertility potential.
-
In Vitro Fertilization (IVF): Enhances the chance of pregnancy through assisted fertilization, especially useful for patients with fallopian tube obstruction or diminished ovarian function.
-
Conceive with donor eggs: Suitable for women with severely impaired ovarian function or poor egg quality. IVF using donor eggs can significantly increase the chances of pregnancy.
Q3. If I can’t get pregnant on my own, can I consider surrogacy?
For patients who are unable to carry a pregnancy themselves, surrogacy is a viable option. In the United States, surrogacy is legal and protected by law.
RSMC provides full-service surrogacy support, including:
-
In-house surrogate database:RSMC has a strictly vetted pool of surrogate candidates, ensuring that each surrogate is physically and mentally healthy and possesses a strong track record of healthy pregnancies and deliveries.
-
Legal and Medical Protection: We provide professional legal consultation and comprehensive medical support to guarantee the legality and safety of the entire surrogacy process.
-
Full-Service Support: From embryo creation, surrogate matching, and pregnancy management to all procedures following the baby’s birth, RSMC offers an all-inclusive, one-stop service.

U.S. Fertility Policies Ensure That Your Frozen Eggs Will Absolutely Be Put to Good Use!
In addition to having the highest IVF success rates in the world, the RSMC laboratory is CPA-certified, and the medical team has 20 to 30 years of extensive clinical experience in IVF and egg freezing. Surrogacy is legal and well-developed in California, and both legislation and public opinion are highly supportive of single individuals and LGBTQ+ people. IVF for single individuals and same-sex couples is both legal and compliant, which is one of the main reasons clients choose to pursue IVF and surrogacy through RSMC. Additionally, undergoing treatment in the U.S. allows you to legally select the baby’s gender—within the bounds of U.S. regulations—based on the priority of the child’s health. All consultants serving the Asian region are full-time employees of RSMC, and pricing is identical to that in the U.S., with no hidden fees—reliable and professional.
RSMC is located in San Diego and Irvine, California, and was established in 1997. With 28 years of clinical experience in reproductive medicine and infertility treatment, we have assembled a team of the top OB-GYN fertility specialists and embryologists in the United States. We also have PhD-level Chinese medical consultants who provide expert guidance and translation, along with bilingual medical staff who specialize in assisting Asian clients to ensure you can proceed with peace of mind. Our clinic is equipped with a CPA-certified professional laboratory, the highest international standard, capable of cultivating high-quality embryos. Our IVF success rate exceeds 80%, and egg donor IVF has a pregnancy success rate of over 87%.
While most surrogacy agencies end their services once the baby is born, RSMC partners with a curated network of service providers. Whether you need assistance with document processing, postpartum care centers, or transporting your baby back home without traveling to the U.S., we are here to help at any time. With extensive cross-border experience, we are able to offer you comprehensive support.
To schedule a free consultation with a U.S. physician or to learn more about pricing and procedures, please contact us via Line / WeChat: rsmctw or WhatsApp: +1 858-342-6046.
Meet Our Doctors
RSMC’s professional medical team in the U.S. consists of leading OB-GYN specialists with over 30 years of experience in reproductive medicine and fertility care.
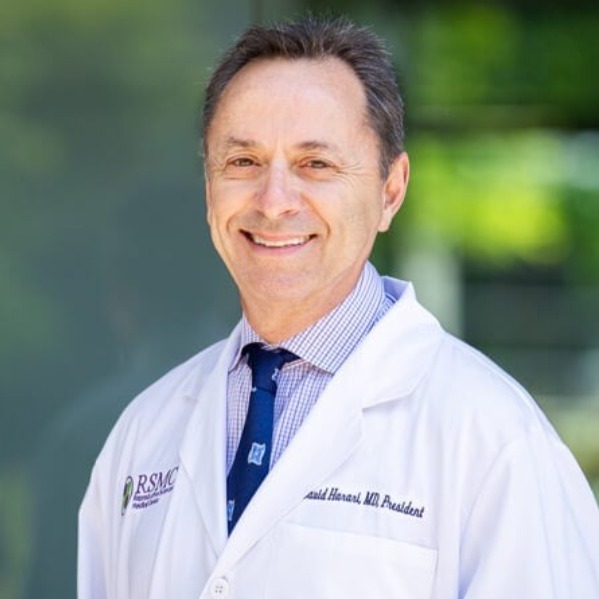
DR. DAVID HARARI
Medical Director of RSMC San Diego
Dr. Harari earned his Medical Doctorate from the University of Georgia Medical Center, completed his internship at the Georgia Medical School, and later finished his residency training at Mercy Medical Center. With over 30 years of clinical experience, Dr. Harari is currently the President of the San Diego Obstetrical and Gynecological Society, which boasts over 400 professional OB-GYN members. Throughout his practice, Dr. Harari deeply respects each patient's personal wishes, providing them with the most professional treatment plans and working collaboratively to help them achieve their goals. He believes in the importance of clear communication and mutual understanding between doctors and patients and is always eager to share his extensive medical experience and offer the best professional advice.
Other
-
2024/11/18ivf
What is a Uterine Polyp? Does It Affect Fertility?



